

Review Article | Open Access Volume 2022 | Article ID 2845902
Alaa Makke, "Vitamin D Supplementation for Prevention of Dental Implant Failure: A Systematic Review", International Journal of Dentistry, vol. 2022, Article ID 2845902, 5 pages, 2022
Academic Editor: Dinesh Rokaya | Received: 25 Oct 2021 | Revised: 27 Dec 2021 | Accepted: 03 Jan 2022 | Published: 12 Jan 2022Abstract
Background. Many factors play a significant role in osseointegration and healing after dental implant insertion and restoration. Some factors are related to dental biomaterials, such as the dental implant, prosthesis, and grafting materials. Other factors can be connected to operator skills and accumulated experience. Local and systemic patient-related factors are crucial in determining the success of the dental implant. Thorough examination and analysis of local factors using available examination tools are vital to prepare the implant candidate for such treatment.
The patient’s systemic condition directly affects the healing of the dental implant. One of the most overlooked systemic factors is the patients’ vitamin D level, which influences bone formation around the implant and subsequent osseointegration. The current review examined the available literature regarding the association between vitamin D supplementation and dental implant osseointegration.
Methods. Data of this review were derived from recent research available on PubMed, Google Scholar, and Scopus. Inclusion criteria were the relation between the vitamin D serum and dental implant osseointegration or failure. The Systematic Reviews and Meta-Analyses (PRISMA) checklist was followed to perform the review. The study’s outcome was the need for vitamin D supplementation to prevent implant failure. Results. Five human studies (including case reports, case series, and retrospective studies) and six animal studies. All included studies discussed the relationship between vitamin D, early dental implant failure, and bone implant contact. Three retrospective studies found no significant relationship between vitamin D supplementation and EDIFs in humans. On the other hand, one retrospective study showed a significant relationship in humans.
A case report and case series claimed that the implant was successfully placed after vitamin D supplementation. A total of four animal studies showed a significant relationship between vitamin D supplementation and osseointegration of the dental implant. Two animal studies showed no significant association. Conclusion. To ensure optimal treatment outcomes, it is recommended to supplement the patient with vitamin D if the serum level is not within the normal range. Further clinical studies and case reports are needed to confirm the association between serum vitamin D levels and osseointegration.
1. Introduction
Osseointegration is the key to dental implant success and is required to achieve direct structural and functional bone formation. For this to occur, many integrated factors should be thoroughly assessed, such as surgical techniques, type of prosthesis, biomaterials, and operator- and patient-related factors 1>. Implant failures are classified according to the timing of the loss to early dental implant failure (EDIF) or late dental implant failure (LDIF). Early implant failure occurs due to improper implant placement and restoration, low bone volume or density, systemic conditions, or smoking 2, 3>.
The primary goal for any oral implantologist is to obtain satisfactory healing and long-term treatment success. Most researchers and manufacturing companies pursue innovations through new implant designs and surface treatment to increase stability and accelerate the osseointegration process. Often, systemic health is a significant factor that is not adequately considered. The human skeleton derives its vitality from key minerals, such as calcium, fluoride, magnesium, potassium, vitamin B6, vitamin D, and zinc 4>. The European Register of Nutrition and Health described 18 items that directly affect bone and teeth, including vitamin D 5>, one of the most necessary micronutrients for dental implant osseointegration. Therefore, adequate exposure to sunlight and optimal dietary habits support the maintenance of satisfactory vitamin D levels 6>.
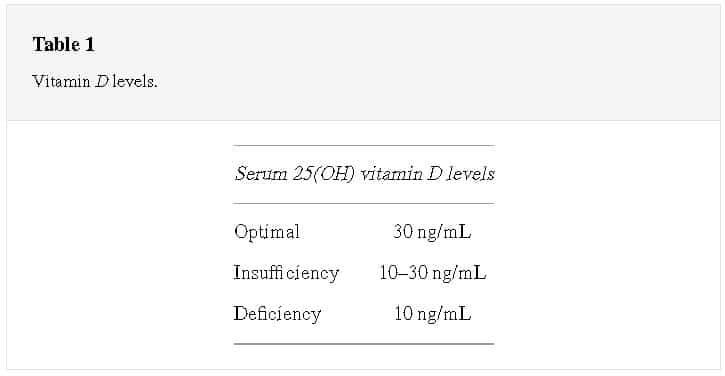
Vitamin D insufficiency is defined as any serum level ranging between 21 and 29 ng/ml, deficiency is when levels are less than 20 ng/ml, and severe deficiency is less than 10 ng/ml (Table 1). Vitamin D3 is the basic form of the vitamin D family, and it is activated by hydroxylation in the liver. Vitamin D stimulates osteoclastic activity and the production of extracellular matrix proteins by osteoblasts. Moreover, it increases calcium absorption in the intestines 7–11>. Some studies proposed that a low vitamin D level might be associated with EDIF 2, 12>. Therefore, the purpose of the current review is to investigate the available literature regarding vitamin D supplementation and dental implant osseointegration.
The most recently published English research was reviewed, including animal studies, in vitro studies, case series, case reports, cohort studies, and clinical studies. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist was followed to perform the review. Data were collected using the following keywords: vitamin D, dental implant, implant failure, osseointegration. A database such as Google Scholar, PubMed, Scopus, or ResearchGate was used to explore recent research. Inclusion criteria were studies investigating the vitamin D serum and dental implant osseointegration or failure. Exclusion criteria were incomplete data and irrelevant or duplicated studies. Data were reviewed according to the patient age and sex of the patient, the year of the study, and the number and location of the study.
3. Role of Vitamin D on Dental Implant OsseointegrationSunlight vitamin D synthesis begins from cholesterol in the skin converted into pre-vitamin D3 and then isomerized to vitamin D3. Subsequently, 25-hydroxyvitamin D3 resulting after vitamin D3 is hydrolyzed in the liver 13>. Primarily, vitamin D stimulates the osteoclastic activity and production of extracellular matrix proteins by osteoblasts and increases the Ca absorption in the intestines 7–11>. Likewise, there is a microbicidal effect on monocytes affected by vitamin D levels, which increase the body’s resistance to bacteria, fungi, and viruses 14>. There was a significant correlation between infection rate and vitamin D levels <20 ng/ml 15>. Therefore, the optimal vitamin D level might be one of the most critical systemic factors in preventing infection and providing an optimal environment for successful osseointegration.
4. Retrospective Studies and Case ReportsA retrospective study on 1,740 implants placed in 885 patients showed no significant relationship between low vitamin D levels and increased risk of EDIFs 16>. In patients with serum levels of vitamin D < 10 ng/ml, there were 11.1% EDIFs before loading the prosthetic part. In comparison, when the serum level of vitamin D was between 10 and 30 ng/ml, the EDIFs was 4.4%, and when the serum level of vitamin D was >30 ng/ml, there was a 2.9% EDIF rate. The retrospective study by Wagner et al. showed a significant and positive effect of vitamin D on marginal bone loss at the mesial and distal aspects of the dental implants 17>.
Similarly, a retrospective study of 1,625 implants placed in 822 patients showed an increase in the incidence of EDIFs in patients with compromised vitamin D levels, but statistically, it was not significant. The study described 9% EDIF for those with a serum level of vitamin D < 10 ng/ml and 3.9% EDIFs for those with a serum level of vitamin D between 10 and 30 ng/ml. Surprisingly, a 2.2% EDIF rate was noted in patients with a serum level of vitamin D > 30 ng/ml 18>.
A case series examined implants that were successfully osseointegrated in two patients with a history of EDIFs after vitamin D supplements 19>. Another case report claimed EDIFs occurred after immediate implant placement due to severe vitamin D deficiency 20> (Table 2).
5. Animal StudiesKelly et al. found exposed implant surfaces in vitamin D-deficient rats and bone fracture between the implant and surrounding bone after 14 days of implant placement when subjected to a lower push-in test and lower bone to implant contact (BIC) 21>. On the contrary, vitamin D supplementation increased bone density by 1.2-fold and osseointegration by 1.5-fold and extrusion force resistance by 2.0-fold in osteoporotic rats. The trabecular bone amount was increased by 96%, and osseointegration was elevated up to 94.4%, while the trabecular number was elevated by 112.5% and 51.8% in connective tissue 22>.
Wu et al. used vitamin D and insulin on diabetic rats to improve osseointegration. The study claimed that bone volume, osseointegration, trabecular bone number and thickness, connective tissue density, BIC, and push-out force were enhanced 23>. Another study on diabetic rats showed no significant effect of vitamin D on osseointegration. In a different study, vitamin D combined with insulin was administered to diabetic rats, and histological analysis was conducted during the third week after implant placement. A BIC level of 44 was measured in the diabetic rats and 57 for rats in the vitamin D + insulin group. Six weeks later, the BIC level was 70 for the control group and 65 for the vitamin D group 5 24>. Dvorak et al. observed no significant rescission of BIC in the medullar and periosteal compartment among rats that received vitamin D in their diet compared to those which did not receive it 25>.
A significant difference was observed when vitamin D supplements were administered to rats with chronic kidney disease (CKD) compared to those with CKD without supplementation. BIC levels were significantly higher among the supplementation group 26> (Table 3).
6. DiscussionThe current review aimed to investigate the association between vitamin D levels and the osseointegration process of a dental implant. The United States Centers for Disease Control and Prevention’s National Health and Nutrition Survey claimed an insufficient intake of vitamin D for more than 25% of the US population. This deficiency is shared outside the US, with more than 2 billion people worldwide also showing vitamin D deficiency. Thus, vitamin D deficiency directly affects the skeleton of the human body, including the jawbone 27>, and therefore, it may play a critical role in dental implant treatment outcomes. Accordingly, a stable vitamin D level will assist in maintaining a healthy body, and ideal daily amounts are 2,000 IU (50 mcg) for most people and up to 4,000 IU 27> during pregnancy.
The current review included five human studies (including case reports, case series, and retrospective studies) and six animal studies. All included studies discussed the relationship between vitamin D, EDIFs, and BIC.
A significant relationship was found between vitamin D and osseointegration in four animal studies when BIC was examined. A lower push-in test was performed 14 days after implant insertion in rats. Kelly et al. found that, after scanning electron microscopy (SEM) analysis, all rats with vitamin D deficiency showed exposed implant surfaces, which occurred because of bone fracture between the implant and the surrounding bone 21>. Likewise, an investigation conducted to determine the effect of 1,25(OH)2D3 on implant osseointegration in osteoporotic rats indicated that vitamin D supplementation resulted in significant bone formation around the implant 22>.
Other animal studies showed that bone volume increased when vitamin D was used with insulin in diabetic rats after implant placement 24>. The mean bone volume and osseointegration outcomes of the studies were very similar to those of healthy rats. Similarly, Liu et al. proved that CKD rats that received vitamin D supplementation showed greater BIC and bone volume than CKD rats that did not receive vitamin D supplementation 23>. The studies, as mentioned earlier, showed the importance of vitamin D supplementation, especially for compromised rats. The findings of these studies demonstrated the significance of supplemental vitamin D in the short- and long-term outcomes after dental implant treatment.
Two animal studies showed no significant correlation between vitamin D supplementation and dental implant osseointegration 24, 25>. Akhavan et al. showed that vitamin D supplementation did not significantly affect osseointegration, although the study did not mention if the experimental rats received diabetes medication 24>. Dvorak et al. showed that there no significant difference when rats were fed a standard vitamin D diet 25>. However, the study did not mention the vitamin D blood levels of the rats after diet administration.
There has been a lack of human studies examining the association between vitamin D serum levels and osseointegration. In 2018, Mango et al. investigated vitamin D serum levels and EDIFs in a retrospective clinical study that included 885 patients, with specified inclusion and exclusion criteria 16>. Their findings showed 35 EDIFs (3.9%) reported, with no significant relationship between the EDIFs and patient gender, smoking, history of periodontal disease, or vitamin deficiency. Three EDIFs were noted in 27 patients with vitamin D serum levels <10 ng/ml, 20 EDIFs in 448 patients with groups of 10–30 ng/ml, and 12 EDIFs in 410 patients with serum levels >30 ng/ml. Limitations of the study included the sample size of the patients with low serum levels of vitamin D and the retrospective design.
One case report found severe vitamin D deficiency correlated with immediate implant placement 20>. A case series confirmed this hypothesis when the implant was successfully osseointegrated after D supplementation, although there was a previous implant failure 19>. Interestingly, the results of the retrospective studies, case reports, and case series concluded that the serum level of vitamin D seems to influence dental implant osseointegration. The limitation of the study includes a limited number of available data and sample size and few clinical studies.
7. ConclusionsAdditional prospective clinical studies and case reports are required to determine the association between serum vitamin D levels and osseointegration. Some studies showed a clear association in terms of osseointegration and EDIFs. Additional studies with specific inclusion and exclusion criteria are necessary to isolate vitamin D levels as the only factor tested. If a patient’s vitamin D level is severely compromised according to the level mentioned in this review, the recommendation is to supplement with vitamin D to ensure optimal treatment outcomes.
Abbreviations| BIC: | Bone to implant contact |
| EDIFs: | Early dental implant failures. |
The data supporting this review are from previously reported studies and datasets, which have been cited.
Conflicts of Interest
The author declares no conflicts of interest.
References
- B. R. Chrcanovic, J. Kisch, T. Albrektsson, and A. Wennerberg, “A retrospective study on clinical and radiological outcomes of oral implants in patients followed up for a minimum of 20 years,” Clinical Implant Dentistry and Related Research, vol. 20, no. 2, pp. 199–207, 2018. View at: Publisher Site | Google Scholar
- F. G. Mangano, P. Mastrangelo, F. Luongo, A. Blay, S. Tunchel, and C. Mangano, “Aesthetic outcome of immediately restored single implants placed in extraction sockets and healed sites of the anterior maxilla: a retrospective study on 103 patients with 3 years of follow-up,” Clinical Oral Implants Research, vol. 28, no. 3, pp. 272–282, 2017.
- View at: Publisher Site | Google Scholar
- O. Buhara and S. Pehlivan, “Estimating the importance of significant risk factors for early dental implant failure: a Monte Carlo simulation,” The International Journal of Oral & Maxillofacial Implants, vol. 33, no. 1, pp. 161–168, 2018. View at: Publisher Site | Google Scholar
- F. Javed, H. Malmstrom, S. V. Kellesarian, A. A. Al-Kheraif, F. Vohra, and G. E. Romanos, “Efficacy of vitamin D3 supplementation on osseointegration of implants,” Implant Dentistry, vol. 25, no. 2, pp. 281–287, 2016. View at: Publisher Site | Google Scholar
- G. Iolascon, R. Gimigliano, M. Bianco et al., “Are dietary supplements and nutraceuticals effective for musculoskeletal health and cognitive function? A scoping review,” The Journal of Nutrition, Health & Aging, vol. 21, no. 5, pp. 527–538, 2017. View at: Publisher Site | Google Scholar
- L. Nastri, A. Moretti, S. Migliaccio et al., “Do dietary supplements and nutraceuticals have effects on dental implant osseointegration? A scoping review,” Nutrients, vol. 12, no. 1, p. 268, 2020. View at: Publisher Site | Google Scholar
- M. R. Brinker, D. P. O'Connor, Y. T. Monla, and T. P. Earthman, “Metabolic and endocrine abnormalities in patients with nonunions,” Journal of Orthopaedic Trauma, vol. 21, no. 8, pp. 557–570, 2007. View at: Publisher Site | Google Scholar
- D. Alkalay, S. Shany, and S. Dekel, “Serum and bone vitamin D metabolites in elective patients and patients after fracture,” Journal of Bone and Joint Surgery British Volume, vol. 71-B, no. 1, pp. 85–87, 1989. View at: Publisher Site | Google Scholar
- H. F. DeLuca, “The vitamin D story: a collaborative effort of basic science and clinical medicine 1,” The FASEB Journal, vol. 2, no. 3, pp. 224–236, 1988. View at: Publisher Site | Google Scholar
- R. Bouillon, W. H. Okamura, and A. W. Norman, “Structure-function relationships in the vitamin D endocrine system,” Endocrine Reviews, vol. 16, no. 2, pp. 200–257, 1995. View at: Publisher Site | Google Scholar
- S. Christakos, P. Dhawan, Y. Liu, X. Peng, and A. Porta, “New insights into the mechanisms of vitamin D action,” Journal of Cellular Biochemistry, vol. 88, no. 4, pp. 695–705, 2003. View at: Publisher Site | Google Scholar
- A. S. Dusso, A. J. Brown, and E. Slatopolsky, “Vitamin D,” American Journal of Physiology - Renal Physiology, vol. 289, no. 1, pp. F8–F28, 2005. View at: Publisher Site | Google Scholar
- D. Apostu, O. Lucaciu, G. D. O. Lucaciu et al., “Systemic drugs that influence titanium implant osseointegration,” Drug Metabolism Reviews, vol. 49, no. 1, pp. 92–104, 2017. View at: Publisher Site | Google Scholar
- B. Lehmann, “The vitamin D3 pathway in human skin and its role for regulation of biological processes,” Photochemistry and Photobiology, vol. 81, no. 6, pp. 1246–1251, 2005. View at: Publisher Site | Google Scholar
- P. T. Liu, S. Stenger, H. Li et al., “Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response,” Science, vol. 311, no. 5768, pp. 1770–1773, 2006. View at: Publisher Site | Google Scholar
- F. Mango, S. Osakoui, A. Paz, N. Mango, and C. Manago, “Low serum level Vitamin D and early dental implant faliure,” Joddd, vol. 12, no. 3, pp. 174–182, 2018. View at: Google Scholar
- F. Wagner, K. Schuder, M. Hof, S. Heuberer, R. Seemann, and G. Dvorak, “Does osteoporosis influence the marginal peri-implant bone level in female patients? A cross-sectional study in a matched collective,” Clinical Implant Dentistry and Related Research, vol. 19, no. 4, pp. 616–623, 2017. View at: Publisher Site | Google Scholar
- F. Mangano, C. Mortellaro, N. Mangano, and C. Mangano, “Is low serum vitamin D associated with early dental implant failure? A retrospective evaluation on 1625 implants placed in 822 patients,” Mediators of Inflammation, vol. 2016, Article ID 5319718, 2016. View at: Publisher Site | Google Scholar
- T. Fretwurst, S. Grunert, J. P. Woelber, K. Nelson, and W. Semper-Hogg, “Vitamin D deficiency in early implant failure: two case reports,” International Journal of Implant Dentistry, vol. 2, no. 1, p. 24, 2016. View at: Publisher Site | Google Scholar
- G. Bryce and N. MacBeth, “Vitamin D deficiency as a suspected causative factor in the failure of an immediately placed dental implant: a case report,” Journal of the Royal Naval Medical Service, vol. 100, no. 3, pp. 328–332, 2014. View at: Publisher Site | Google Scholar
- J. Kelly, A. Lin, C. J. Wang, S. Park, and I. Nishimura, “Vitamin D and bone physiology: demonstration of vitamin D deficiency in an implant osseointegration rat model,” Journal of Prosthodontics, vol. 18, no. 6, pp. 473–478, 2009. View at: Publisher Site | Google Scholar
- C. Zhou, Y. Li, X. Wang, X. Shui, and J. Hu, “1,25Dihydroxy vitamin D3 improves titanium implant osseointegration in osteoporotic rats,” Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology, vol. 114, no. 5, pp. S174–S178, 2012. View at: Publisher Site | Google Scholar
- Y.-y. Wu, T. Yu, X.-y. Yang et al., “Vitamin D3 and insulin combined treatment promotes titanium implant osseointegration in diabetes mellitus rats,” Bone, vol. 52, no. 1, pp. 1–8, 2013. View at: Publisher Site | Google Scholar
- A. Akhavan, Z. Noroozi, A. Shafiei, A. Haghighat, G. Jahanshahi, and S. Mousavi, “The effect of vitamin D supplementation on bone formation around titanium implants in diabetic rats,” Dental Research Journal, vol. 9, no. 5, pp. 582–587, 2012. View at: Publisher Site | Google Scholar
- G. Dvorak, A. Fügl, G. Watzek, S. Tangl, P. Pokorny, and R. Gruber, “Impact of dietary vitamin D on osseointegration in the ovariectomized rat,” Clinical Oral Implants Research, vol. 23, no. 11, pp. 1308–1313, 2012. View at: Publisher Site | Google Scholar
- W. Liu, S. Zhang, D. Zhao et al., “Vitamin D supplementation enhances the fixation of titanium implants in chronic kidney disease mice,” PLoS One, vol. 9, no. 4, Article ID e95689, 2014. View at: Publisher Site | Google Scholar
- G. Isaia, R. Giorgino, G. B. Rini, M. Bevilacqua, D. Maugeri, and S. Adami, “Prevalence of hypovitaminosis D in elderly women in Italy: clinical consequences and risk factors,” Osteoporosis International, vol. 14, no. 7, pp. 577–582, 2003. View at: Publisher Site | Google Schola

